Guest Blog Post: Maureen Tyra, LICSW, ACP Coordinator – How North Memorial is Promoting Advance Care Planning in Minnesota
While our advance care planning efforts focus primarily on the 65+ audience, we realize we need to move these conversations upstream by encouraging every adult to have a health care directive in place by the time they’re 30. But the struggle continues to revolve around how best to “normalize” these conversations.
During preventive care education and office visits, we talk about family health risks, lab results, and very private health matters — why isn’t advance care planning among the routine doctor/patient conversation? At North Memorial, we’re working to change that.
 We first partnered with Respecting Choices®, an internationally recognized, evidence-based model of advance care planning (ACP) that creates a culture of person-centered care to honor an individual’s goals and values for current and future health care needs. As part of the first phase, we conducted leadership engagement training, and some outreach to assisted living communities and nursing homes.
We first partnered with Respecting Choices®, an internationally recognized, evidence-based model of advance care planning (ACP) that creates a culture of person-centered care to honor an individual’s goals and values for current and future health care needs. As part of the first phase, we conducted leadership engagement training, and some outreach to assisted living communities and nursing homes.
From there, we dedicated a full year to exploring what an ideal ACP process would look like across our entire system, working with Epic to make sure electronic health records (EHRs) would be consistent and reliable. The process in every setting is fully integrated, and we are now working on additional process improvements, such as improving the ability to know about and honor POLST* orders, and reporting on ROI to improve reimbursement levels (e.g., extra hospital days, costly care that patients don’t want, stress on families and health care workers…).
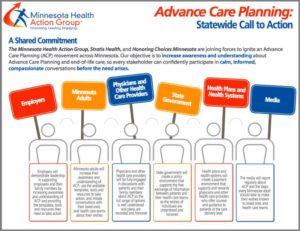
I see great value in the Advance Care Planning Call to Action issued by the Minnesota Health Action Group, Honoring Choices Minnesota, and Stratis Health. The Action Group adds an important new dimension by rolling out the initiative through employers who have a real opportunity to make change happen through very large and very diverse employee audiences. By involving so many stakeholders, organizations of all types and sizes can actively contribute to promoting the importance of advance care planning.
The value of the Minnesota Movement will be enhanced by uncovering and dispelling myths, normalizing advance care planning as part of preventive care, using a light touch — even humor — to educate, and helping people see that having the conversation is empowering…it gives you rights; it doesn’t take them away.
North Memorial Initiatives
- In the hospital setting: A health care directive questionnaire is built right into Epic, which all nurses are expected to follow upon admission (with 90 percent compliance). If the patient has a health directive, staff members ask if the hospital has a copy and, if not, the patient receives a self-addressed, stamped envelope to mail in a copy. All patients without an advance care directive are given a packet of information, and a full-time person and trained volunteers are available to answer questions.
- In the ambulatory setting: In settings such as primary care and specialty clinics, nursing homes, and assisted living facilities, the recommendation is for patients without an advance care directive to be asked about completing one once a year, and those who have an advance care directive to be asked if they have updates once a year. All clinics have at least one person who is a trained facilitator. An important next step is to improve the process of what to do if patients don’t have a health care directive.
*POLST, or Physician Orders for Life Sustaining Treatment (a doctor’s order to follow patient wishes): The national POLST paradigm is an approach to end-of-life planning based on conversations between patients, loved ones, and health care professionals. It is designed to ensure that seriously ill or frail patients can choose the treatments they do or do not want and that their wishes are documented and honored. Included in a POLST are a patient’s wishes about things like CPR, medical interventions, and artificially administered nutrition (i.e., “tube feeding”). Health care professionals recommend posting the POLST somewhere obvious in the patient’s care setting in case emergency personnel are called.